Event: Mind-Reading 2017
A Forgotten Episode of International Health by Dora Vargha
The Establishment of the World Health Organization
The establishment of the World Health Organization is no doubt a crucial and fundamental moment in the history of international (and global) public health. The leadership, ideas and early decades in the unfolding Cold War can be assembled through biographies of Director-Generals, the Organizations own chronicle of its first decades and through histories of malaria eradication. However, certain equally important aspects of the early years of the WHO, like the sudden exit of the Soviet Union and Eastern Europe shortly after the establishment of the organization merit little more than a mention in these histories.
The Socialist Bloc and the Missing History of the WHO
Andrija Stampar, key member of the League of Nations Health Organization (LNHO) and president of the First World Health Assembly, and Ludwik Rajchman, director of the LNHO and founder of UNICEF. Often seen as a politically homogeneous area under complete Soviet control in the postwar era, Eastern European countries have not been considered to have agency in international health during the Cold War.
But the history of international and global health has a lot to gain by including the Socialist Bloc in the picture. This unexplored history points to questions whether international health always happens within organizational structures of international agencies and through philanthropic entities such as the Rockefeller Foundation; what the stakes were in this Cold War divide in the formative years of the WHO; and the extent to which we can talk about a unified response within the Socialist Bloc to diplomatic and public health challenges in their time outside of the organization.
Socialist Networks and International Public Health
Considering alternative international public health, in this case socialist networks, is crucial in getting a complete picture of postwar international public health and its effect on modern global health. The historiography of internationalism has been going under a rapid change by including alternative internationalisms and focusing on socialist exchange in ideas, practices and knowledge. Much of this new research has addressed issues of development, culture and education. Many have called attention to Eastern Europe’s role in transcontinental collaboration and have placed contributions to postcolonial projects in focus. With some notable exceptions, such as Young-Sun Hong’s work on East German development projects, or Ana Antic’s research on transcultural psychiatry in Yugoslavia, health has mostly escaped the attention of these new histories.
Through the lens of Hungary, the last country to re-join the WHO in 1963, my research aims to put Eastern Europe in the focus of international health inside and out of the World Health Organization. I seek to explore what happened to international health in Eastern Europe, outside of the purview of the usual suspects: international agencies and non-governmental organizations, like the Rockefeller Foundation, how complete was the break with liberal internationalism and what, if anything, took its place.
It was not long after Eastern European states successfully joined that the Soviet Union decided to leave the WHO. The Russians were not very eloquent in their reasoning, they cited the mammoth bureaucracy, high member fees and the political influence of the United States in the WHO. The exit of the Soviet Union, followed by the whole Socialist Bloc challenged the proclaimed universality of the newly formed WHO and the centrality of technical expertise in opposition to political allegiance. The quick deterioration of the East’s relationship with the organization seems to fit neatly into a narrative of the escalating Cold War and increase of the Soviet Union’s hold on Eastern Europe. However, when inspected in detail, the reasons for the exit of these countries was more complex and had to do as much with expectations of what an international health agency should do, as with foreign policy.
Grievances towards the WHO
 |
| Dr Josepf Plojhar, (right), Minister for Health, Czechoslovakia. Also pictured, Tadeusz Michejda (left), Minister for Health, Poland; Luitpold Steidle (right), Minister for Health, GDR. Berlin, 14 September 1950. Bundesarchiv. Bild 183-T00826 |
Socialist countries did not have their own penicillin plants back then, they had to import the needed amount for hard currency from the West. The Czechs, in order to become independent, purchased a whole penicillin plant from the Americans before the political turn of February 1948, which according to the contract the US had to deliver in two installments. The first one arrived, but the second one, which was to be delivered after the political turn, was held back by the Americans. Father Plojhar, wearing priest’s attire, asked the delegation of the United States in front of the Assembly, why they had not honored the contract. The American delegate, putting aside all civility (and with the knowledge of the subservient voting machines behind its back) just briefly said: "Contract, no contract, you turned socialist, you get nothing!" The president of the assembly then put the Czechoslovak question to vote, and apart from the 5 yes votes of the socialist countries present, the issue was overruled by the majority. The vassals "voted well" - it was a real American decision. I wouldn’t have thought that professional issues, what’s more, questions of health can be distorted so under political duress.1
While Plojhar’s speech does not appear in the minutes, the American delegate, Leonard A. Scheele Surgeon General referred to it and dismissed the claim by stating that the equipment in question is not necessary for the production.
Attributing Eastern European countries’ decision to leave solely to Cold War political alignments would be a mistake, however. Recent research on the years of communist takeover has shown that the relationship of the Soviet Union and Eastern European countries was a complex one and certain aspects of that relationship were very much open ended. We cannot readily assume a master plan from the Soviet side, with which Eastern European states quickly fell in line with. Moreover, while the overwhelming influence of the United States in the WHO and pressure from the Soviet Union no doubt playing an important part, countries like Hungary had other, substantial reasons for discontentment.
Second World Health Assembly
| Second World Health Assembly, Rome, 13 June to 2 July 1949: Decisions and resolutions: plenary meetings verbatim records: committees minutes and reports: annexes. Courtesy of WHO: IRIS |
However, there were problems: several Eastern European delegates criticised the WHO for its one size fits all approach. Apart from issues with access to penicillin, the Czechoslovak delegate called on the WHA to rethink the universality of certain public health issues and instead, consider health priorities on a national level. The Hungarian Health Minister, István Simonovits pointed to the fact that while Hungary considers fellowships to be crucial as a form of pursuing international public health, many of its fellows are regularly denied entry visas to WHO member states and are therefore unable to attend conferences they are invited to. Simonovits also considered visiting lecturers to be less useful for Hungarian public health: “Even the best lecturer was hardly more useful than a good article, because in many cases the lecturer had no knowledge of our special local problems.”
The criticism of several of the Eastern European delegates point to a different expectation of the tasks and responsibilities of international health organizations. In the late 1940s the countries in question were still in a horrid state, their hospitals bombed, medical equipment seized or destroyed, with extreme housing problems and crumbling infrastructure. In countries with extreme shortages of medication, physicians and buildings fit to house patients, and with no access to the Marshall Plan or other forms of aid, the policy of the WHO to give technical assistance instead of material aid seemed pointless, offensive even. As Plojhar, the Czechoslovak delegate put it: "It is more urgent for us to dispose of some public-health problems than to receive good advice."
 |
| The buildings of the Foreign Ministry and War Office in Budapest, 1949. Photograph by Carl Lutz. Foto:Fortepan/Archiv Für Zeitgeschichte Eth Zürich / Agnes Hirschi. Photo ID: 105808 |
Withdrawal from the WHO
The second World Health Assembly was the last one that Eastern European countries attended for almost a decade. Romania, Albania, Poland, Czechoslovakia and Hungary left the organization in 1950. Some of the delegates, like Plojhar warned of this possibility at the Second WHA in 1949. But perhaps the withdrawal was not a clear choice. Instead of issuing a warning, the Hungarian delegate used his speech to plead for the inclusion of socialist approaches to public health, and to remedy the situation that caused the Soviet Union to leave the organization.
The withdrawal of such a substantial number of countries from the WHO placed the question of membership into focus and pointed to broader questions of supranationality and state sovereignty. The WHO navigated its practice among two legal school of thoughts: one of which considers such an international organization to be supranational, making a unilateral withdrawal impossible once a member voluntarily joined, and another considering membership in the international organization to be dependent on its alignment with foreign policy. The United States favoured the latter interpretation, its Congress upholding the right to withdraw within a year of joining the WHO. The organization itself adopted a position of compromise between the two schools, introducing “inactive membership” for withdrawing states. This latter solution also helped save the international organization some embarrassment, when the Soviet Bloc exited the WHO.
Not only did the practice of international public health in Eastern Europe continue with the budding socialist internationalism within the Bloc, but countries like Hungary continued to participate through interaction and collaboration with the West. Being out of the WHO, divided by the Iron Curtain also did not mean that the region was isolated in terms of international health. If we shift our focus from viewing internationalism in public health from the perspective of international organizations and governments, and turn to the agents of internationalism themselves, we find that the sites of international collaboration in public health were as varied as the people acting as internationalists. Families and virologists, hospital directors and religious scholars were actively involved in shaping international collaboration in research, treatment and access to technology.
Decentering Narratives of Internationalism and Global Public Health
Geographically and conceptually de-centring narratives of internationalism and global public health, especially ones tied to the Cold War, is crucial for a nuanced understanding of this formative era. By bringing Eastern Europe into the focus and considering alternative internationalisms, new faces, practices and relationships become visible, which, in the end, can help us piece together a very messy and often confusing picture of international and global health in the 20th century.
Dora Vargha
 |
| Dr Dora Vargha |
Dr Dora Vargha is a lecturer in the Medical Humanities at the University of Exeter. Previously, she has held research fellowship positions at the Max Planck Institute for the History of Science, Berlin and at Birkbeck, University of London. She is an acclaimed authority on the history of global health and biomedical research in the Cold War era with a particular focus on Eastern Europe.
Dora's work has been widely published in leading peer-reviewed journals including Contemporary European History, and Bulletin of the History of Medicine. She has recently completed the manuscript for her forthcoming monograph Iron Curtain, Iron Lungs: Governing Polio in the Cold War which explores a series of polio epidemics in Hungary in the context of international Cold War politics. She has recently embarked upon a new research project, for which she received a Wellcome Trust Seed Award, titled, 'Socialist Medicine: An Alternative Global Health History'.
Dora is the recipient of many scholarly awards including the J Worth Estes Prize from the American Association for the History of Medicine and the Young Scholar Book Prize from the International Committee for the History of Technology. She is the founding editor of and a contributor to the Central and Eastern European History of Medicine Network Blog. Dora is also a collaborating member of the Reluctant Internationalist research group, a Wellcome-Trust funded project that is researching the history of public health and international organisations.
1 Tibor Bakács, Egy Életrajz Ürügyén (Budapest: Kossuth Könyvkiadó, 1978).↩
Alcohol, Medicine and Irish Society, c.1890-1970 by Alice Mauger
Wellcome Trust Medical Humanities Fellowship
A Wellcome Trust Postdoctoral Fellowship has been awarded to Dr. Alice Mauger. Her three-year project on ‘Alcohol, Medicine and Irish Society, c.1890-1970’ is being hosted by the UCD Centre for the History of Medicine in Ireland (CHOMI). It is mentored by Dr. Lindsey Earner-Byrne, Deputy Head of the School of History, UCD and sponsored by Associate Professor Catherine Cox, Director of UCD CHOMI.
 The project explores the evolution of medicine’s role in framing and treating alcoholism in Ireland. It assesses the period from the 1890s, when acceptance of inebriety as a disease led to the creation of the short-lived inebriate reformatories, to the 1970s, when dedicated rehabilitation facilities were formed in response to the rising number of psychiatric patients diagnosed with alcohol-related illnesses.
The project explores the evolution of medicine’s role in framing and treating alcoholism in Ireland. It assesses the period from the 1890s, when acceptance of inebriety as a disease led to the creation of the short-lived inebriate reformatories, to the 1970s, when dedicated rehabilitation facilities were formed in response to the rising number of psychiatric patients diagnosed with alcohol-related illnesses.Until now, the history of medicine has offered little reflection on the relationship between medicine and alcoholism in Ireland. While the ubiquitous “drunken Irish” stereotype, still prevalent today, has been evaluated from several viewpoints, we have yet to discover how international and Irish medical communities interpreted, informed and absorbed this label. By investigating care in asylums and inebriate reformatories, along with medical debates and shifting government policies, the project questions how the exchange of medical, government and lay ideas came to shape understandings and experiences of alcoholism in Irish society.
 |
| Still image from the television show, 'Home Truths', featuring a segment on alcoholism, RTÉ, 7 December 1966. Image courtesy of the RTÉ Stills Department. |
Context
Despite the popularity of temperance and pioneer movements in Ireland since the mid-nineteenth century and high levels of abstinence reported into the 1950s, the Irish have traditionally been viewed as being especially prone to alcoholism. Irish emigrants were persistently portrayed as heavy drinkers, while the emergent Irish nationalist movement sought to associate abstinence with patriotism – some prominent members even claiming that the British encouraged Irish drinking to demoralise the population. In these ways, alcoholism was inextricably linked to theories or fears of Irish degeneration.
This project questions the extent to which enduring stereotypes of the Irish as violent and drunken permeated contemporary medical conceptions of alcoholism, and whether this in turn influenced political and lay interpretations.
Internationally, several works have focussed on shifting medical concepts of addiction. This project situates Irish therapeutic and diagnostic trends alongside those in other western countries, including Britain, America and Australia. It also seeks to inform the extensive literature on the history of psychiatry, particularly degeneracy and ethnicity, and related discourses in Irish social history covering themes such as poverty, violence and the family.
Aims
The project aims to make a significant contribution to the medical humanities, exploring historical sources to better understand and contextualise Irish society’s relationship with alcohol. In doing so, it hopes to inform present-day social and cultural concerns.
Keys findings from the project will be presented in a monograph, journal article and a series of posts on the CHOMI blog, as well as papers given at relevant forums.
In 2019, Alice will organise an interdisciplinary workshop on ‘Alcohol, Medicine and Society’ at CHOMI, inviting policy makers and academics from Ireland and overseas. A call for papers for this event will feature on this blog.
Alice has also planned a one-month knowledge exchange to the Centre for History in Public Health in the London School of Hygiene and Tropical Medicine to engage with prominent experts on addiction history including Professor Virginia Berridge and Dr. Alex Mold.
Biography
 |
| Dr Alice Mauger |
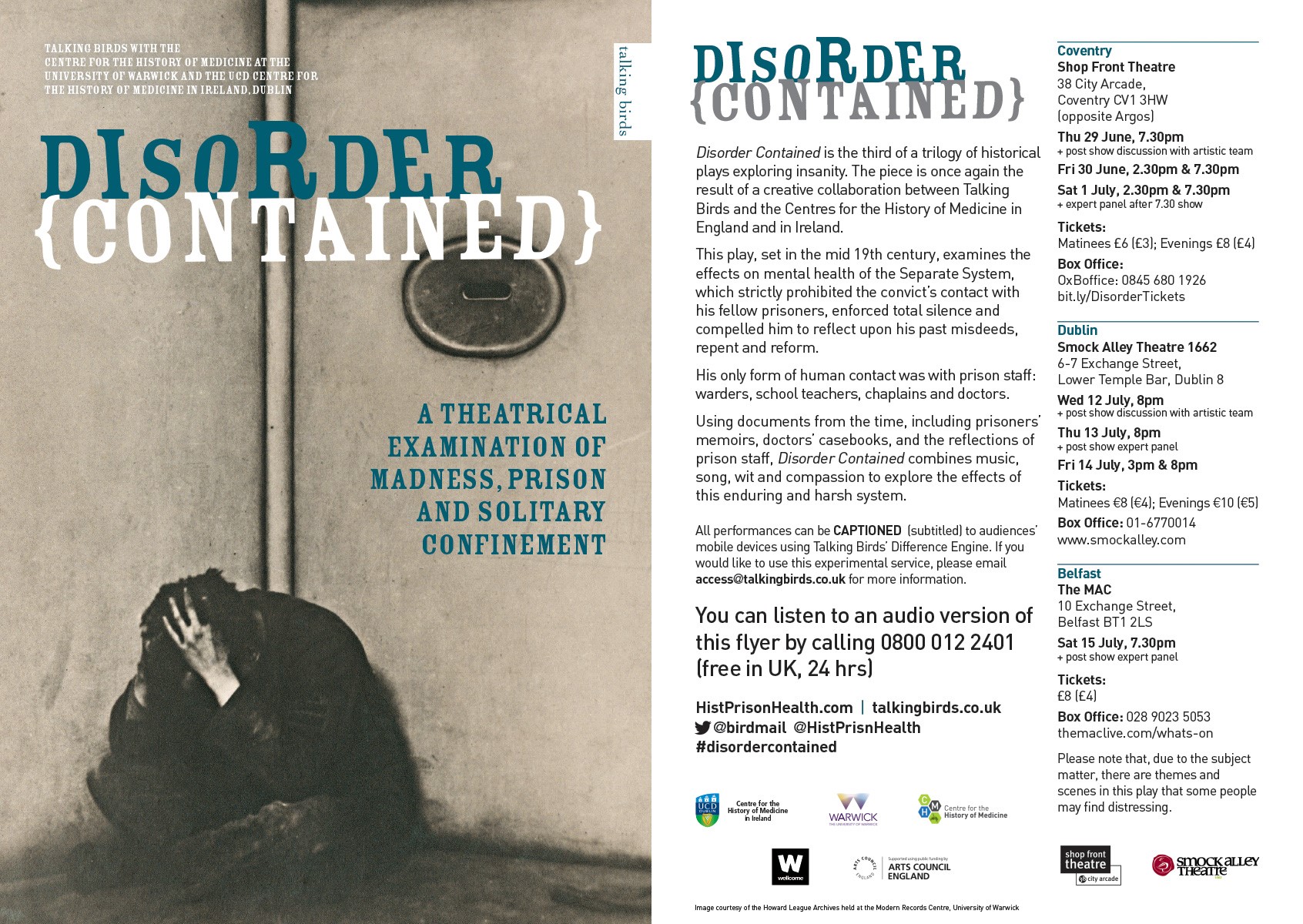
Disorder Contained: Theatre Performances, Coventry, Dublin, Belfast
A Theatrical Examination of Madness, Prison and Solitary Confinement
Disorder Contained: A theatrical examination of madness, prison and solitary confinement is a major public engagement activity for the Wellcome Trust funded project Prisoners, Medical Care and Entitlement to Health in England and Ireland 1850-2000. It draws on the work of Associate Professor Catherine Cox (UCD) and Professor Hilary Marland (Warwick) and forms the final part of The Asylum Trilogy exploring various aspects of the history of mental health.The production, created with Talking Birds and to be performed in Coventry, Dublin, Belfast, and London during 2017, will be accompanied by Expert Panel Discussions as well as Post-show Artistic Conversations which will be recorded along with the performance.
Book Tickets
- Coventry from 29 June - 1 July: Book tickets
- Dublin from 12 - 14 July: Book tickets
- Belfast on 15 July: Book tickets
See Also
- Show announcement
- Press release
- Theatre dates and tickets
- Audio flyer
- Reflective blogs (on translating historical research into accessible theatre)
- Disorder Contained: Reading
An Tobar: a Two-day Workshop on Sacred Springs and Holy Wells
Waterford Museum of Treasures, 26-27th June 2017
Most languages encode the sacrality of fresh water springs: for example, Heilige Quelle (German), source sacrée (French), kisima kitakatifu (Swahili) or ayazmalar (Turkish). India has its hallowed pools and sacred wells or kūpas, Mexico has its holy water aguajes and Mayan cenotes. Shinto kami (spirits) dwell in Japanese springs, while spring wells on China’s Mount Lao grant Taoist pilgrims a thousand lives. Thousands of holy wells exist across Roman Catholic, Protestant, and Orthodox Europe: Austria has 467, Denmark has 650, and Russia has nearly 3500. Wales has at least 1,179, Scotland has perhaps over 1000, and a conservative estimate for England’s holy wells is 2,000. The National Monuments Service of the Republic of Ireland documents the early nineteenth-century locations of over 2900. We can perhaps agree with the Roman writer, Servius, who claimed: “nullus enim fons non sacer” (there is no spring that is not sacred)!
The social significance of sacred water bodies and their associated traditions is now an emerging subject of study. One area where Irish scholars in particular are making great advances is the medical and curative dimension to these sites. These papers represent exciting new research taking place across Ireland into the various ways holy wells and their landscapes have played and continue to play a role in approaches to health and wellbeing.
Healing Waters and Therapeutic Landscapes
North Leinster Holy Wells: A Medical Geography – Ronan Foley, Maynooth University
One of the primary reputations of holy wells is their function as curative sites. Medical/health geographers are equally interested in the idea of therapeutic landscapes, places or spaces with established reputations for health and healing. With increased access to spatial information on the location of holy wells, and a parallel development in the mapping of folklore sources about specific cures, it has become possible for the first time to create a medical geography of holy wells in Ireland. Sources vary from traveller’s accounts and local historical sources to material from the Schools Collection and more recent surveys and ethnographic site visits. This paper describes the spatial distributions of specific cures in North Leinster as a representative location and considers the extent to which some wells had quite specific named curative powers, while others were panaceal. In addition, the location of the different cures across time and space will complement ongoing work at Trinity College Dublin on scientific testing of the waters to see if local geographical conditions can in part explain their distribution. Finally, the use of GIS and other geo-spatial mapping approaches identify the ongoing ways in which holy wells databases can be developed to promote the preservation of their narrative histories and ongoing curative performances.
Dr Ronan Foley is a Senior Lecturer at the Department of Geography at Maynooth University, Ireland. He has written extensively in the broad area of therapeutic landscapes, including Healing Waters: Therapeutic Landscapes in Historic and Contemporary Ireland (2010). He is currently the PI on an Irish Environmental Protection Agency project on Green/Blue Spaces and Health & an advisory partner on an ESRC project at the University of Exeter on Sensing Nature.
Tobair beannaithe agus ‘an leigheas’: Holy Wells and ‘the cure’ in 20th Century Ireland – Carol Barron, Dublin City University
The Schools Manuscript Collection of 1937-38, housed in the Folklore Department in UCD is believed to be the largest single medical folklore collection in Europe, and offers us a unique insight into the believes, practices and rituals surrounding ‘the cure’ and Holy wells in 20th Century Ireland. This paper examines a subsection of over 7,500 ‘cures’ sampled from the Schools Manuscript Collection from each barony of each of the 26 counties of Ireland, of which over 250 ‘cures’ are specific to Holy wells. This shared socio-cultural phenomenon is critically examined from a folkloristic/anthropological perspective, focusing on the specific disease states and their cultural importance to the health of Irish society at the time of recording and through history.
Dr Carol Barron is a lecturer in the Department of Nursing and Human Sciences at Dublin City University. She received her PhD in Anthropology from NUI Maynooth and her research focusses on child health. In particular, she has conducted extensive investigation into the use of Irish folk cures.
Well-being: Holy Wells as Emergent Therapeutic Spaces – Richard Scriven, University College Cork
Applying the concept of therapeutic landscapes to holy wells, this paper examines these sites as spaces of wellbeing that are forged through the interactions of people and place. Holy wells can be appreciated as sources of health offering spiritual and emotional support to individuals and communities. These experiences are generated in the meeting of bodies and practices, location and materials, and beliefs and emotions. Within these processes, well-being emerges with the site rather than being taking from it: there is a ‘taking place’ of health and wellbeing. Drawing on my fieldwork at holy wells across Munster, I explore the practices and meanings that contribute to the creation of these spaces of wellbeing and offer speculations on further engagements with this arena.
Dr Richard Scriven is an Irish Research Council Government of Ireland Postdoctoral Fellow in the Department of Geography, UCC. His research examines pilgrimage in contemporary Ireland as a socio-cultural phenomenon.
Holy Wells: The Evidence from Ulster – Finbar McCormick, Queen’s University
The experience of attending holy wells was composed of two main components, health and penance. While the curative nature of the wells is generally emphasised, the great majority of those who attended sites were not suffering for sickness or disability, - “every face beaming with the glow of health” as one observer noted. The main aim was to ensure the maintenance of good health for the coming year. This aspect of the ritual often involved washing or bathing in the well’s waters something that has for the most part disappeared in modern holy well rituals. The earliest place-name evidence for holy wells in Ulster and elsewhere, dating to the early Medieval period, indicates their association with health. It is likely that the penitential aspect of the wells is a later development. This paper considers a chronology for understanding the layered meanings of holy well rituals in Ulster.
Dr Finbar McCormick teaches Archaeology at Queen’s University Belfast and has recently been researching and excavating Struell wells in County Sown. Struell contains the most extensive set of buildings associated with a holy well in Ireland and can be documented back to the early Medieval period.
Further Details
Dr Sinead McCann: Receives Two Arts Council Awards
Sinead, a noted Irish visual artist, received these awards in her role as a Public Engagement Officer on the Wellcome Trust Senior Investigator Award project, Prisoners, Medical Care and Entitlement to Health in England and Ireland, 1850–2000. This project is led by co-Principal Investigators Associate Professor Catherine Cox, Director of UCD CHOMI, and Professor Hilary Marland, Director of the Centre for the History of Medicine, University of Warwick.
Inside Health: Thinking about Prisoners' Right to Healthcare
The Trial
When Does The Air Matter? by Janet Greenlees
Air Quality and the Working Environment
In this month's blog post Dr Janet Greenlees, Senior Lecturer at Glasgow Caledonian University, looks at the history of industrial air quality and considers how it has variously been considered a worker's health, community health, and economic concern.
When Does Air Matter?
 |
| Men and women weaving at the White Oak Mill in Greensboro, NC, 1909. Courtesy of the National Museum of American History. |
An Air Laden with Dust and Dirt
Worker Fatigue and Factory Ventilation
 |
| The Boott Cotton Mill of Lowells, Massachusetts. Courtesy of the Lowell Museum Collection. |
Cotton Dust Inhalation
 |
| Interior of a Lancashire Cotton Mill with Mill Workers at their Machines, Lancashire, c. 1890. |
Managing the Health Impact of the Working Environment
Janet Greenlees
 |
| Dr Janet Greenlees |
Lecturer/Assistant Professor in the History of Medicine
Lecturer/Assistant Professor in the History of Medicine (Modern)
University College Dublin - UCD College of Arts & Humanities
| Location: | Dublin |
| Salary: | €52,325 to €82,267 £46,379.78 to £72,919.74 converted salary* |
| Hours: | Full Time |
| Contract Type: | Permanent |
| Placed on: | 4th April 2018 |
| Closes: | 20th April 2018 |
| Job Ref: | 010231 |
Abortion and Symphysiotomy in Ireland
Law and Gender in Modern Ireland
 |
| Lynsey Black and Peter Dunne (eds.), Law and Gender in Modern Ireland: Critique and Reform(Hart Publishing, 2019 |
We are currently in the midst of a ‘Decade of Centenaries’ in Ireland. For anyone working broadly in the field of gender, it is also clear that we have lived through a decade of reckoning. As editors of the recently published Law and Gender inModern Ireland: Critique and Reform(Hart, 2019), one of the key challenges has been to present the current legal regime in its historical context. As the book started to take shape, it became clear that the intersection of medicine, gender and the law was an essential part of this story. Within the collection, chapters by James Gallen (Dublin City University) and Máiréad Enright (University of Birmingham), which deal with symphysiotomy and abortion respectively, have provided insight into the role that gender ideologies played in medical practice in post-independence Ireland. Their chapters outline the prevailing historical context in which these medical procedures became emblematic of Catholic conservative Ireland, and the contemporary redress and reform which have attempted to resolve these wrongs.
Catholic society
 |
| The march of the Archbishops - Bishops etc., outside Pro Cathedral, Congress 1932, Dublin City. Eason Collection, National Library of Ireland. |
Symphysiotomy
Abortion
Historical abuse
Survivors of symphsiotomy
Repeal of the 8th Amendment
 |
| A mural outside the Bernard Shaw pub in Portobello Dublin depicting Savita Halappanavar and calling for a yes vote in Ireland's referendum to remove the 8th Amendment. Photo by Zcbeaton, Creative Commons Licence. |
Continuing concerns
Lynsey Black
 |
| Dr Lynsey Black |
Irish Medical Responses to Problem Drinking from Institutionalisation to Public Health: Part I
After over 1,000 days of debate, in October 2018, the Irish government passed the Public Health (Alcohol) Bill. The Act will introduce minimum unit pricing as well as rigorous regulations surrounding advertising, sponsorship, sale and supply. Under this legislation, Ireland may become the first country in the world to attach stark health warnings to alcohol products. Billed as the first time the Irish state has legislated for alcohol as a public health issue, the Act is intended to significantly alter the culture of drinking in Ireland. While unsurprisingly the subject of extensive lobbying from the drinks industry and other stakeholders, the measures have gained overwhelming support from the Irish medical profession. The Bill’s tortuous passage is therefore a reminder of Ireland’s ambivalent and complex relationship with alcohol. This relationship is deeply embedded in Irish politics, culture and society and has a very long historical lineage.
A ‘Disease Concept’ of Inebriety
 |
| Ephraim M. Cosgrave (1853-1928). Courtesy of the Royal College of Physician of Ireland Heritage Centre |
Perhaps the most ardent Irish medical commentator on alcohol in this period was Ephraim MacDowel Cosgrave, a physician at several Dublin hospitals who would later become president of the Royal College of Physicians (RCPI). For Cosgrave, the creation of institutions specially designed for the ‘control of inebriates’ would be the answer to Ireland’s ‘drink question’.1
Cosgrave was not alone in promoting this approach. Inebriate homes are said to have originated in the United States in the first half of the nineteenth century and by 1870 had begun to appear in Britain. Cosgrave’s stance mirrored British developments, where under the guidance of leading inebriety expert, Dr Norman Shanks Kerr, medical practitioners were canvassing for the system’s expansion. Yet, in Ireland, many doctors continued to recommend alternatives ranging from committal of drunkards to lunatic asylums to their detention at home by physical force.2
Despite the almost draconian nature of these suggestions, such attitudes did not apparently extend to alcohol itself. Reacting to proposals to further restrict pub opening hours at weekends, in 1895 a contributor to the Dublin Journal of Medical Science declared:
We object to the grandmotherly legislation and coercion. The liberty of the subject is sufficiently restricted already, and the patience with which millions of law-respecting citizens tolerate the curtailment of their personal liberty, lest a weak brother should offend, is a marvellous testimony to our inborn respect for law. Restrictions and pledges cannot create an Utopia.3
Such claims diverged significantly from the now commonly accepted ‘disease view’ of inebriety, which saw alcohol as an inherently addictive substance, which put anyone who drank at serious risk of losing control over their habit. In Ireland, at least some doctors were openly contesting further restrictions, a fact which lends further weight to traditional portrayals of more permissive popular attitudes towards drunkenness in Ireland.
Institutions for Inebriates
 |
| Painting by patient in St Patrick’s Hospital, Dublin (1905). Source: E/137 Case Book, Males, St. Patrick’s, p.32. |
Instead, lunatic asylums became the principal treatment centres for problem drinkers. By 1900, 1 in 10 people admitted to Irish asylums were sent there due to ‘intemperance in drink’. This trend gained increasing attention among psychiatrists, not least because of mounting uncertainty as to whether excessive drinking could actually cause mental illness. Some asylum doctors recognised intemperance as a manifestation of an existing mental disorder, others cited adulterated alcohol as a cause and still more believed that the habitual drunkard produced offspring liable to insanity. This latter claim was to be expected, given that alcohol and degeneration were now strongly linked in discussions of the alleged increase of insanity both in Ireland and overseas.
Given the influx of these cases, the Irish psychiatric community were soon called upon to respond. In 1904, delegates at a conference of the British Medico-Psychological Association in Dublin were confronted with evidence of the ‘disastrous effects everywhere observed’ of drink. Reporting on this event in the association’s official journal, the writer proclaimed:
It may cause some searching of conscience to ask whether our profession as a whole, and particularly our speciality, have up to the present taken a sufficient leading part in the holy war against alcohol. It is high time for our Irish colleagues to make themselves heard upon this subject, when in at least one asylum, one third of the male admissions are attributed chiefly to this cause.4
This battle cry reverberated with the temperance rhetoric of the day, a movement which boasted strong support from some Irish asylum doctors. Meanwhile, members of the wider medical community showed signs of absorbing, and even propagating, the Nationalist-toned temperance claim that sobriety held the key to Irish independence. In 1904 a reviewer for the Dublin Journal of Medical Science decreed:
One of the heaviest blows which a patriotic Ireland could possibly inflict on its neighbouring British rulers would be given by taking the pledge all round – old and young – and keeping it! Why, we often say to ourselves, do not patriotic politicians utilise this fact?5
In spite of calls to engage in the ‘holy war against alcohol’, Irish psychiatrists made little comment in the ensuing decades. Soon after, discussion of the links between alcoholism and degeneration became seriously compromised by new scientific studies which found no evidence that alcoholism in a parent gave rise to mental defects in their children.
As will be discussed in the next instalment of this series, after the First World War, there was a shift in focus towards alcohol and later, problem drinkers, with the eventual acceptance of a new ‘disease view’.
Alice Mauger
 |
| Dr Alice Mauger |
Alice has published on the history of psychiatry in Ireland including a full-length monograph: The Cost of Insanity in Nineteenth-Century Ireland: Public, Voluntary and Private Asylum Care (Palgrave Macmillan: 2017), which is available via open access and in hardcopy.
Who’s to Blame?: Inquests into Convict Deaths in Mountjoy, c.1868-1900
 |
“Death of a Convict in Mountjoy Prison”, Evening Telegraph (1 October 1895). Newspaper image © The British Library Board All rights reserved. With thanks to the British Newspaper Archive. |
Inquests
In late 1800s Ireland, when someone died an investigation into their death was carried out at the coroner’s discretion. Generally, inquests only happened in cases of suspicious or unusual deaths, and the last attending medical practitioner, or any other local medical professional, was consulted. The medical community in general took these inquests quite seriously, and the ‘Principal Laws’ that governed United Kingdom medical professionals included a section on proper inquest conduct. These rules emphasized that medical officials giving evidence should be honest and accurate as their testimony was usually very influential.2
For general medical practitioners, these inquests could be stressful affairs. Depending on the outcome, the inquest could either enhance their professional reputation or destroy it. The same held true for PMOs, who had the added weight of also being responsible for protecting the prison’s reputation.3 Prior to 1877, prisoner death inquests were only called if the coroner felt one was necessary. In 1877, with the passing of the General Prison (Ireland) Act, inquests became mandatory in the event of a prisoner’s death. As a result, the number of inquests increased and PMOs ended up in front of a jury more frequently defending themselves and the prison.
The PMOs
For information on prisoner death inquests, I mainly looked at Irish newspaper articles concerning the Dublin convict prison Mountjoy and two PMOs that worked there in the late 1800s: Dr James William Young and Dr Patrick O’Keefe. Young served at Mountjoy as a PMO from 1867-83. O’Keefe succeeded Young as head PMO at Mountjoy and served there from 1883-c.1907. Both Young and O’Keefe were highly educated individuals with multiple medical degrees who made careers out of working for the Irish prison system as medical officers.4 As PMOs, Young and O’Keefe were in charge of the general health of prisoners. They assigned diets, determined whether or not prisoners were suited for punishment or labor, and treated inmates’ specific aliments, among other duties.
Newspaper reports of the coroner’s inquests reveal that while Young and O’Keefe faced scrutiny in these hearings, Mountjoy itself received the majority of the blame in prisoner deaths. Coroner’s inquests in the late 1800s largely ended up being arenas where juries, coroners, and even the PMOs themselves, questioned and critiqued the Irish penal system’s care of prisoners in Mountjoy.
Death by Natural Causes
In other cases, ultimately both the prison and PMOs were cleared of blame, but during the trial there were debates over the various parties’ culpability. This is perhaps due to the general sense of skepticism when it came to Mountjoy that Sullivan mentioned in his letter at the beginning of this post. We can see evidence that others shared Sullivan’s concern over Mountjoy through the kinds of questions juries asked of the defendants, which often demanded that the PMOs explain in detail the care provided to the deceased. Some of the newspapers also reported that the juries were critical of the PMOs going into the inquests. After the death of a prisoner in 1868, for example, the jury was reportedly suspicious of Young from the outset. However, in this case they ultimately decided that he was not to blame.7
The testimonies that Young, O’Keefe, and other prison officials provided also suggest they were well aware of the public’s suspicion surrounding Mountjoy and tried to assuage any such fears. In 1883, during the inquest into Michael Watters’ death, Young, O’Keefe, and Kelly, another medical practitioner, all agreed that ‘death was not attributable to punishment or any form of ill-treatment’, thus contesting the notion that the prison’s disciplinary methods could be responsible for Watters’ death.8 In an 1886 case, the jury found that James Davies’ died of natural causes after a very laudatory testimony from the city coroner concerning the treatment of prisoners in Mountjoy. The coroner was adamant that Davies did not die as a result of neglect, saying that once a prisoner became ill ‘all his crimes appeared to be forgotten by the prison officials, who did everything for his comfort … they always have the best medical treatment’.9 Given the suspicion surrounding Mountjoy at the time, this praise was quite possibly an active attempt to combat the concern over inadequate prisoner care.
PMO Blamed for Convict Death
During Lynagh’s inquest, Young explained that he was treating Lynagh, but thought he was improving. As a result, Young initially declined to send Lynagh to the prison hospital. Ultimately, the jury blamed Young for Lynagh’s death, arguing that Lynagh should have been sent to the hospital much sooner. They also specifically called out Young, saying he ‘might be more attentive to extern patients’.10
Or Was the Prison Really at Fault?
While the jury in the Lynagh case firmly held that Young was to blame, the nationalist newspaper The Nation and the official Commissioners’ Report presented slightly different takes on Lynagh’s death. Both addressed the jury’s critique of Young, but argued that Lynagh’s death was not actually Young’s fault. One month after the inquest, the Commissioners released their report exonerating Young. They recognised the jury’s verdict, but said that Lynagh’s death was inevitable and ‘that the man was not neglected during his illness by Dr Young or the other officers of the prison’.11 Notably, while defending Young, they also declined to assign any blame to the prison system.
The Complicated Case of Johanna Hayes
In 1870, Young was dragged back into the spotlight with the death of Johanna Hayes in Mountjoy Female prison. During the hearing, Young reportedly testified that after entering the prison Hayes’ health began declining, and he recommended that she be released from prison with respect to her failing health. However, this recommendation was not heeded, and Hayes remained in prison where she died. In contrast to the Lynagh case, here the jury lauded Young for his attempts to aid Hayes and get her released. Interestingly, the jury did not directly blame the prison system, despite the penal system’s denial of Hayes’ release on medical grounds. The jury did note, however, that Hayes died as a result of her being in prison.14 This conclusion suggests the jury found the prison partly to blame, but not wholly at fault as it had not actively contributed to Hayes’ death.
While this trial ended relatively well for Young and the prison, not everyone agreed with the jury’s take on the events. Like the jury, Sullivan, the aforementioned nationalist journalist, did not blame Young, although he was skeptical of him. Rather, Sullivan railed against the Irish penal system in a letter to the city coroner, which was eventually published in the newspaper The Warder. In this letter, Sullivan addressed his preference for Young’s predecessor, Dr Macdonnell, and basically called Young a government lackey. He also commented on the testimonies presented in the Hayes trial. In particular, Sullivan disliked the reliance on Young’s deposition, saying the jury held ‘a suspiciously laudatory protestation’ of Young, and that it was ‘very likely all true; but methought the jury did protest too much’.15
Sullivan’s issue with the jury’s praise was further illuminated during a libel trial that resulted from the publication of this letter. During that libel trial, Mr Butt, speaking for defendant Sullivan, argued that the jury’s praise was for the benefit of Young and the prison system:
Then came the [Hayes] inquest, when Dr. Younge [sic] whitewashed off the black cloud of censure passed on him at the first inquest [Lynagh’s case in 1868] … was it very strange if Mr. Sullivan should say this was an attempt to prop up a new system, in which Dr. Younge [sic] was to be praised for his exertions?16
In House Complaints
Critiques of the prison system were not unusual in inquests, and as we have already seen there was an established suspicion surrounding prisoner deaths and the prison system’s level of blame. Prison outsiders, such as juries, coroners, and journalists like Sullivan, used these inquests to question the prison system. Likewise, prison insiders also utilized inquests to critique the prison, and Young and O’Keefe occasionally provided testimonies that called out the prison’s operation and treatment of prisoners.
The other issue highlighted in the newspaper coverage was the implementation, or lack thereof, of night nursing in Mountjoy. The coroner implied that Connor would have been better cared for had there been a better nursing system in place. When the coroner asked O’Keefe for his take on the system of night nursing, O’Keefe initially refused to give an opinion. After the coroner pressed, O’Keefe relented replying ‘Well, I think it might be improved’.18
Following the death of a convict in 1878, Young testified that he had done what he could for the patient in the prison cells, but chose not to send the prisoner to the hospital. This decision was vastly unpopular with the jury who heavily questioned Young’s decision. Young claimed that the convict was not sent to the hospital because of ‘the small hospital accommodation and heat of the weather … the accommodation [in hospital] was insufficient’.19 Using the public forum of the inquest, Young aired his complaint about the prison hospital and argued its inadequacy directly contributed to the convict’s death.
While both Young and O’Keefe clearly critiqued Mountjoy and the ways in which the prison was run, these criticisms were not perhaps without ulterior motive. Going into these inquests, the juries were already suspicious of Young and O’Keefe and the care they provided. As a result, it is possible that O’Keefe and Young highlighted the poor night nursing and hospital accommodations respectively as a way to transfer the blame from them to the prison at large. In both of these cases as well, neither O’Keefe nor Young were found at fault for the prisoner’s death.
Conclusions
Annika Liger
Acknowledgements
A Prescription for Change: Training a Doctor in Nineteenth and Twentieth-Century Ireland
A Case of History Repeating Itself
Status Update
 |
| 'A poor apothecary in a cart being drawn by his servant are overtaken by a wealthy couple in a horse-drawn carriage with a seat at the back for their servant'. Credit: WellcomeCollection. CC BY |
The decade or so preceding James’s entry into medicine saw many attempts to professionalise the sector. In trying to move medicine away from being considered a trade to a profession, this naturally had a knock on effect towards the social standing of the doctor. Generally, and particularly before the middle of the nineteenth century, medicine had a tripartite structure and like most structures, was hierarchical in nature. At the top there was the physician, followed by the surgeon with the apothecarist sitting on the bottom rung of the ladder. The three enjoyed differing levels of social status. Alongside the orthodox or regular practitioners, were the unorthodox practitioners or "quacks". These included druggists, bonesetters or any member of the medical community that occupied the fringes of society. The medical marketplace was already overcrowded, especially in England, and having to compete for patients alongside unqualified "quacks" naturally created some anxiety for the trained practitioner.
The Medical Act, 1858 attempted to alleviate some of these concerns. The Act tried to regulate the education and training of doctors and required all practicing members to sign the registry of the General Medical Council (GMC). While it differentiated between regular and irregular practitioners by only allowing fully trained and qualified ones to sign the register, the Act failed to prevent "quacks" from actually practicing. Members of the public were still unlikely to be able to discern between the two. The Act went some way towards professionalising medicine by trying to control entry and setting a standard of training. This meant that registered practitioners could distance themselves from tradespeople by charging for a service rather than a commodity. However, the Act was considered a failure for many orthodox members of the community as it still meant they had to jostle their way through a saturated market rife with "quacks".1
The Price of Education
 |
| 'A foppish medical student smoking a cigarette, a tankard is on top of his medical books; denoting a cavalier attitude (1854)'. Credit: WellcomeCollection. CC BY |
Upwardly Mobile
The Family Business
The Spectre of Emigration
Out at Sea
 |
| 'Naval officers and men on a ship, dressed in the uniform of nine labelled ranks of the Royal Navy'. Credit: Wellcome Collection. CC BY |
The Export Market
The More Things Change…
So if today’s doctor is overworked, underpaid, and under-respected, who would want to join such a profession? Well apparently, quite a lot of people. Places to study medicine in Irish universities are still some of the most competitive, typically requiring some of the highest CAO points. The introduction of the Health Professions Admissions Test (HPAT) some years ago attempted to ensure that well rounded candidates were offered places rather than just those that achieved the highest academic scores. School leavers and even mature students are clearly not deterred despite the various challenges – new and old – that beset the medical profession. Like James and Gerald, many could be following an already established family path into the profession. It is likely that for many, having to leave Ireland upon graduating is seen as an exciting opportunity rather than enforced emigration. Rather than being seen as a badge of social standing, there is also the possibility that an offer to study medicine is viewed as a mark of intellectual status. It is well known how hard a secondary school student must work to earn enough Leaving Certificate points to be offered a place. To actually complete the five to six years of medical training is definitely a remarkable achievement. For some, perhaps medicine is just in the blood; a path they were destined to follow, neither a trade nor a profession but simply a vocation.
Natalie Baldwin
Acknowledgements
Irish Medical Responses to Problem Drinking from Institutionalisation to Public Health: Part II
Read Part I here.
A New 'Disease View'
Alcoholism and Mental Hospitals
Dr John G. Cooney
Too often doctors have allowed their view of alcoholics to be distorted by emotional factors. Commonly their own subconscious fears regarding alcoholism have been projected on to their alcoholic patients. If one is to treat alcoholism successfully whether in hospital of in general practice one must feel as well as believe that the alcoholic is ill and suffering from a disease just as surely as a diabetic is suffering from his excess blood sugar.3
Resistance to the Disease View
One of the great difficulties in this country was that alcoholism was not accepted as an illness. It still carried a social stigma, a rather foolish way of looking at a serious disease. The basic illness was often hidden under other names for face-saving thus there were no reliable figures for alcoholism.4
Social and Cultural Factors
 |
| Campaign Poster for Public Health (Alcohol) Bill, 2015. With thanks to Alcohol Action Ireland |
A Public Health Approach to Alcohol
Alice Mauger
 |
| Dr Alice Mauger |
Now Enrolling for 2020/2021: MA in the History of Welfare and Medicine in Society, School of History, UCD
MA in the History of Welfare and Medicine in Society
 Medicine, illness and welfare occupy a central place in all our lives. The MA in the History of Welfare and Medicine in Society is designed to enable you to understand the place of medicine and welfare in society and history (c.1750-1980) and engage with critical debates through various media including film, literature, and art, amongst others.
Medicine, illness and welfare occupy a central place in all our lives. The MA in the History of Welfare and Medicine in Society is designed to enable you to understand the place of medicine and welfare in society and history (c.1750-1980) and engage with critical debates through various media including film, literature, and art, amongst others. Your fellow students will be from diverse academic backgrounds and the MA is popular among healthcare professionals keen to understand the historical contexts that shaped current practices and systems.
Your fellow students will be from diverse academic backgrounds and the MA is popular among healthcare professionals keen to understand the historical contexts that shaped current practices and systems.Why do this MA?
 |
| Assoc Prof Catherine Cox, Director, UCD Centre for the History of Medicine in Ireland |
Further Details
Former MA Students
- David Durnin, The Irish Medical Profession and the First World War (Palgrave Macmillan, 2019).

- David Durnin and Ian Miller (eds), Medicine, Health and Irish Experiences of Conflict, 1914–45(Manchester University Press, 2016).
Our community of graduate scholars continues to grow. Posts by our most recent graduates, based on their MA research include:
- Natalie Baldwin, ‘A Prescription for Change: Training a Doctor in Nineteenth and Twentieth-Century Ireland’.
The Historian’s Kaleidoscope – Making Sense of Medical History in Times of a Pandemic
Trying to make sense of COVID-19 is to look through a kaleidoscope. Within its brief existence, the virus has revealed the incredible complexity of interspecies relationships, economic interdependencies, health system designs, international relations, the many fallouts of the climate emergency, and differing cultural perceptions of disease and biomedicine. It has also unleashed a storm of attempts by historians, social scientists, and public commentators to make sense of the present against the backdrop of previous epidemics and pandemics.
Critics were of course right to highlight that it was too early to provide grand analyses and wrong to make facile comparisons to earlier pandemics. Nobody can accurately predict how interactions between this novel pathogen and its human hosts will evolve and it will likely take decades to retrospectively unpick the complex biosocial interactions that brought us here. However, history is also not as speechless as some seem to imply. While I would distrust anyone proposing a definite analysis of COVID-19, I would be similarly wary of those waiting for the elusive point when current events have ‘safely’ become history.
The COVID-19 pandemic is a biological and social event that is the result of contingent emergence. However, it is playing out within the structural constraints of a human and environmental playing field that was shaped over decades – if not centuries. Historians are uniquely placed to appreciate both the contingency of SARS-CoV-2 and to analyse its pandemic playing field. The relevance of such analyses for decision-making and public discourse is great. I have plenty of colleagues whose excellent work on vaccines, public and global health, infectious disease, mental health, and civil emergencies makes them ideally placed to provide critical context for varying policy responses. Scholars of the medical humanities can also highlight implicit biases and shaky data underpinning some of the epidemiological, behavioural, and economic models guiding current policy. By looking back at previous pandemic or epidemic events, some may even be able to make educated guesses about likely social flashpoints, governance problems, finance bottlenecks, and ethical dilemmata. None of the colleagues I know would make the claim that historical analysis holds universal answers. However, I think that many of them would be comfortable saying that decontextualized policymaking and public debates can be just as flawed – and that expertise from the medical humanities should be represented in official expert bodies.
Reflecting on my own work on antibiotics, laboratory surveillance, and infectious disease control, I have become keenly aware of the kaleidoscopic qualities of the current crisis. All of my research fields have been affected. COVID-19 has accelerated many of the structural constraints that have long prevented equitable and unbiased health provision, international coordination, and global solidarity. However, it has also provided interesting points of departure.
Writing about change, challenges, and prospects in the areas I know best has aided my own historical sense-making and prompted useful exchanges with other disciplines. Together with colleagues from the biomedical and environmental sciences, I have drawn on historical precedents to warn about the likely rise of antibiotic use to deal with bacterial superinfections and resulting selection for antimicrobial resistance (AMR). However, we were also keenly aware that the unprecedented global sharing of scientific information about COVID-19, formation of patent pools, and mobilisation of public funds may also point to new solutions for the long-standing ‘empty pipeline’ problem for antibiotic development. With collaborators from the social sciences, I have reflected on the chequered past of human infection studies in accelerating vaccine development but also exploiting marginalised and colonial populations. We warned that the race for effective SARS-CoV-2 vaccines and the growing tendency to ‘offshore’ trials necessitated a new international framework for infection studies. I was also honoured to reflect on how contagious disease can bring out the best and worst in societies with my former PhD supervisor. Interviews with talented and genuinely interested journalists have also allowed me to stress how the history of drug and vaccine development makes it clear that ensuring equitable access must be at the forefront of current decision-making.
None of these points are particularly revolutionary and I do not pretend to be able to offer a comprehensive interpretation of an unfolding global crisis from the desk in my bedroom. It is, however, clear to me that COVID-19 is rapidly changing the fields I study and the way I see their history. Although I may only be able to see individual pieces of this vast kaleidoscope of change, the time to critically reflect on these changes started in January 2020. To publish these reflections is to stimulate debate, add a critical longitudinal and structural take to public sense-making, and – in my case – to optimistically push for some good things to come out of this global event.
Claas Kirchhelle
Through the Archives: Community Doctors of the Past
In this blog post, Simone Doyle, a student on UCD's MA in History of Welfare & Medicine in Society, explores the career of Dr Neil John Blayney (1874-1919) using archival material donated to the Royal College of Physicians of Ireland's Heritage Centre.
Doctors in Obscurity
Several notable figures tend to dominate our discussions of doctors in the past – Hippocrates, Joseph Lister, Louis Pasteur, John Snow. In Ireland, Francis Rynd (inventor of the hypodermic syringe), and fellow Wexford man, Arthur Leared (inventor of the binaural stethoscope), are arguably our most famous medical men. But what of the lives of the less prominent doctors who served their communities, counties, and country, upheld their Hippocratic oath and were respected members of the medical community? Thanks to material donated to the archives of the Royal College of Physicians of Ireland (RCPI), as well as the work of academics and students studying the history of medicine, and avid amateur historians, many formerly forgotten members of the medical profession are now being rescued from obscurity and having their stories told. This article will discuss one such doctor, Neil John Blayney (1874-1919), and his career in Maryborough County Infirmary, Queen’s County (now County Laois), made possible due largely to the archival material donated to the RCPI by his grandson, Neil Brennan.
 |
| Postcard image of Queen's County Infirmary (early 20th Century) |
Maryborough County Infirmary was established in 1808.[1] By 1836 it housed 868 patients, well above its original capacity of fifty-five. Maryborough was something of an institutional town as it comprised not only the Queen’s County Infirmary and dispensary but a district lunatic asylum (now St. Fintan’s Hospital) and a county gaol (now Portlaoise Prison) that contained eight prison wards (six for men, two for women), nine solitary cells and a prison infirmary.[2]
Neil John Blayney (often referred to as “N J” in newspaper entries for the period) assumed the position of Surgeon and Physician in 1900, after working as the resident surgeon in the Mater Hospital in Dublin and the Mater Infirmorum, Belfast between 1897 and 1899. His appointment was complicated by a local conflict surrounding the previous Physician, a Dr David Jacob’s retirement and his replacement by his son, Dr W.G. Jacob. This appointment was challenged by the Infirmary management, and, after a lengthy campaign, W.G. Jacob was dismissed by the Queen’s County Board in October 1899 and replaced by Blayney.[3] W.G. Jacob challenged this decision in the courts, with Blayney named as co-defendant in the proceedings that ran until 20 February 1900, after which he was confirmed as the surgeon and physician for the Infirmary. Blayney in 1904 described this situation as ‘a period of exceptional difficulty and excitement’.[4]
References from his colleagues prior to his appointment in Maryborough are glowing: ‘he was remarkable for diligence, good conduct and ability’; ‘a highly qualified and competent surgeon…deserving of any position of public trust’; ‘he will, I am confident, be found eminently suitable and give entire satisfaction’.[5] Blayney seems to have lived up to the reputation that preceded him. Father Connolly, a member of the Infirmary Board claimed that ‘nobody could be more attentive or successful than Dr Blayney…in his treatment of them’.[6] At least one of his clients (Major J. Duffield) can be seen to concur, writing to personally thank Dr Blayney and his staff for their swiftness in dealing with ‘the child of a widow … in my charge … who contracted scarlatina … thus preventing the spread of the infection’. As a show of gratitude, Major Duffield donated funds towards the running of the Infirmary.[7]
“Body-snatching”, Suicide and Strychnine
Blayney’s position carried with it a slew of responsibilities, some similar to the work of a modern GP, along with additional duties more conventional for the time. Of the latter, there was his involvement in the training of Voluntary Aid Detachment Nurses during the First World War, giving classes for groups associated with the Irish Volunteers, Cumann na mBan and the Irish Red Cross, and his work on promoting information around the fight against tuberculosis (see below).[8]
His more traditional responsibilities included being attendant to the last moments of many locals and people in surrounding areas, as documented in reports of coroners’ inquests. He assisted a workhouse doctor, Dr McCann in Mountmellick in attempting to save a farmer who had attempted suicide by ‘slicing his own throat’ according to news reports.[9] He gave testimony in the case of Matthew Costigan, a man who died of apparent alcohol-related injuries whose body had been returned to the family by police without the Coroner’s permission, an action which could have resulted in imprisonment for the person blamed for wrongful removal.[10]
Perhaps the most curious of these reports is that on the death of twenty-one-year-old Mary McEvoy. Mary, who had been in apparently good health, died with such suddenness that Dr Blayney at first suspected she may have been poisoned and suggested that the Coroner order a post mortem. At the inquest, however, Blayney changed his opinion, deciding that ‘the only poison could have been strychnine, and since then I have concluded that it could not have been strychnine’. Nevertheless, a post mortem was ordered, performed by Blayney and Dr W.G. Jacob, his one-time opponent. In the end, a brain haemorrhage was cited as the cause of Mary’s death.[11]
Operating Theatre
Given Dr Blayney’s surgical background, it is no surprise that he was among those who advocated for the addition of a proper operating theatre to the infirmary. Management Committee reports reflect just how long and arduous this process was. The first request for funds from the public appear in 1905; by 1907, the probable cost of £200 had yet to be raised, and the theatre remained unsatisfactory (Blayney reportedly said he would ‘be ashamed to show the place to another surgeon’); and the final payment for the work on the theatre was made in April 1911.[12]
Welcome Home Sanatorium
The late nineteenth century and early decades of the twentieth century saw a marked rise in tuberculosis cases. This epidemic had a higher mortality rate than that from other diseases at the time and was attributed to one in every 8.5 deaths in Ireland.[13] The establishment of sanatoria in Germany in the mid-nineteenth century for the treatment of tuberculosis signalled the beginning of a movement of specialised sanatoria building worldwide in the late nineteenth and early twentieth centuries, which had migrated to Ireland by the 1890s.[14]
 |
| Opening Ceremony of Queen's County Sanatorium (Dr Blayney situation on balcony on furthest right) |
Career Conflicts – Local to National
 |
| Dr N.J. Blayney outside Maryborough Infirmary |
In 1908, a dispute was reported between Dr Blayney and other members of the Management Committee over the appointment of nurses. After the resignation of the two former infirmary nurses some months prior, an advertisement was published to fill the vacant positions. Dr Blayney had, without notifying the Board, changed the advertisement’s wording so that it required nurses to have ‘the necessary certificates, as directed by the Local Government Board’. When pressed on why this was necessary when many nurses in private institutions were able to practice without these certificates, Dr Blayney was reported to have said that ‘for the status and dignity of the institution, no nurse should be under the standard laid down by the local government boards’, and that if possible, he would prefer an even higher standard. The Committee Chairman in particular pushed back against this and argued that they should proceed to elect new nurses based on the previous, unaltered advertisement. Despite Dr Blayney’s protest, the election of new nurses was postponed, and the advertisement re-printed with his qualification clause removed.[19]
A larger conflict emerged between Dr Blayney and some other doctors in the area – including Dr T. F. Higgins, the county Coroner, who was a rival applicant for the Medical Advisership position Dr Blayney eventually took up (under the Insurance Act of 1911) in July 1913.[20] On 30 July, Higgins and ten other area doctors co-signed a letter expressing their dissatisfaction with Blayney taking up the post: ‘We express the strongest disapproval of … Dr. Blayney … accepting Medical Advisership … and we call on said doctor to resign, and failing to do so, we decline to have any medical consultations with these officials until they have resigned.’[21]This caused some severe issues for Dr Blayney – the doctors refused to send patients to the Infirmary, or to supply assistance to him on operations, leading to their cancellation. One patient, according to members of the Management Committee, was kept in hospital ‘and fasting’ for a week without being sent for operation because Dr Blayney could not get any of the doctors to assist him. The gravity of the matter was summed up by one of the Committee Members: ‘they have a grievance in legislation, and they want the poor, infirm and suffering people of the county to suffer by that’.[22]
The biggest conflict of Dr Blayney’s career came in November 1903, when he resigned from the Queen’s County Branch of the Irish Medical Association. In a letter to Dr Dunne of the Queen’s County Medical Association, printed in the Leinster Express and elsewhere, Dr Blayney affected his resignation by harshly criticising the Association’s motives for demanding £200 per year for all dispensary medical men and four guineas a week for locums, claiming it showed an ‘evident tendency … by … the association to try and drag the dispensary system into the control of the Civil Service’. He further criticised the Association’s election policy for dispensary doctors, citing a case in Ballyroan in which of the two candidates who presented, only one was qualified for the position. He seemingly insinuated that this candidate was prevented by the Association from presenting himself and warned that if this were allowed to happen elsewhere ‘we would have medical men, appointed by the guardians more or less against their will, who might not be suitable to fill their position, nor might their election be approved of by the majority of the people’. Dr Blayney finished by saying:
It does not resound to the credit of … the association … when we find them trying to prevent the representatives of the people from exercising the authority vested in them.[23]
The version published in the Leinster Leader was accompanied by commentary that suggests Dr Blayney’s letter was ‘bound to exercise a profound influence on the course of the medical controversy’.[24] This certainly seems to have been the case, considering the level of backlash towards Dr Blayney from his colleagues.
In the 14 November issue of the Leinster Express, Dr Higgins criticised Blayney’s worries about dispensaries being put in control of the Civil Service by directly referencing his ascension to the position in Maryborough: ‘Under the civil service system, the best man should be appointed … according to merit. Is that objectionable to Dr Blayney? If so, it means that gratitude to those, who, under a different system, placed him in the County Infirmary, has prejudiced his mind.’[25]
Blayney’s act of protest was dealt a further blow by a letter to the Irish Times from Secretary of the Irish Medical Association, Dr Thomas Gick (reprinted in the Express). The letter stated that despite Dr Higgins’ claim that he had been crucial in formulating the policies of the Queen’s County Branch, Dr Blayney had never actually been a member of the Irish Medical Association, and therefore ‘could not resign that which was not in his possession’.[26]
That Dr Blayney’s career and relationship with his colleagues, particularly Dr Higgins, continued to operate successfully after these clashes suggests that the assessment of Blayney by his peers, infirmary colleagues and patients as an upstanding and consummate professional was almost certainly an accurate one.
Simone Doyle
Simone Doyle is a student on UCD's MA in History of Welfare & Medicine in Society.
Acknowledgements
I would like to thank the following people:
Dr Catherine Cox for her support, kindness, and guidance throughout my studies. To Dr Elizabeth Mullins for inviting me to lecture sessions and talks relevant to my research. Mr Neil Brennan for his insightful talk about his grandfather Dr Blayney and for lending his permission to use his photographs in this blog. To Ms Harriet Wheelock of the RCPI for supplying me with the archival material used. To Dr Alice Mauger for editing, notes and advice on the piece. And finally, to my partner and my mother for their constant support over the course of my studies.
[1] Samuel Lewis, A Topographical Dictionary of Ireland (London, 1837), Accessed at: https://www.libraryireland.com/topog/M/Maryborough-East-Maryborough-Queens.php
[2] Lewis, A Topographical Dictionary of Ireland.
[3] Neil J. Brennan, Opening Dusty Boxes: The Life of a County Surgeon in Edwardian Ireland(Carrigtohill, 2019), 27-8.
[5] M.A. Boyd to N.J. Blayney, 11 November 1898 (RCPI Blayney Collection, Item 63); Charles Coppinger to N. J. Blayney, 20 November 1898 (RCPI Blayney Collection, Item 64); Daniel McDonnell to N.J. Blayney, 30 November 1899 (RCPI Blayney Collection, Item 73).
[10] Leinster Express, 27 April 1912.
[11] Leinster Express, 22 March 1902.
[12] Nationalist and Leinster Times, 28 October 1905; Leinster Express, 1 December 1907; Nationalist and Leinster Times, 1 April 1911.
[13] Alan Francis Carthy, The Treatment of Tuberculosis in Ireland from the 1890s to the 1970s: A Case Study of Medical Care in Leinster (PhD Thesis, National University of Ireland Maynooth, 2015), 1.
[14] Carthy, Treatment of Tuberculosis, 25, 49.
[15] Leinster Express, 2February 1909.
[16] Leinster Express, 29 June 1912.
[21] Dr E.F. Hogan, Dr T.F. Higgins et al to N.J. Blayney, 30 July 1913 (RCPI Blayney Collection, Item 42).
[22] Leinster Express, 31 January 1914.
[24] Leinster Leader 7 November 1903.
[25] Leinster Express, 14 November, 1903.
[26] Leinster Express, 14 November 1903.
[27] Leinster Leader, 14 November 1903.
[28] Leinster Leader, 14 November 1903.
The Eminent and Amiable Doctor Mills
In the late summer of 1830, Dr Thomas Mills of Dublin travelled to Paris with his wife Augusta and sister Kitty. Despite concerns about Thomas’ health, the trio enjoyed a stimulating time meeting friends and seeing the sites of Paris. They stayed at the centrally-located Hôtel des Îsles Britanniques, beside Place Vendôme and Jardin des Tuileries, and the two women experienced the delights of shopping at the vast and glittering Palais Royale. Thomas was more keen to attend political talks and consult with fellow medics. In a letter to his brother back in Dublin,[1] Thomas wrote that he ‘had the good fortune’ to hear General Lafayette, Lafitte and Dupin – all radical, libertarian leaders of the Paris Revolution that had taken place only five weeks earlier.[2]
Who was this Thomas Mills whose ‘heart was pleased’[3] to hear the leading liberal, republican thought-leaders of Paris? There are huge gaps in what we know of the man, and much of the information we have on Mills is drawn from his public profile as a physician. However, we get glimpses of his personal life and private thoughts in a series of letters he wrote from the Armagh and Down countryside, mostly in summer 1805. The letters provide insight into Mills’ personal values and political beliefs as well as presenting acute observations of the lives of people of County Down. The letters are now held in the Royal College of Physicians archive, as part of the Kirkpatrick Collection.[4]
Thomas Mills, Physician ([1773]-1830)
 |
| Figure 1 Portrait of Thomas Mills by Martin Cregan 1788-1870, Royal College of Physicians of Ireland Ref 1850.3, reproduced under Creative Commons Licence CC BY-NC-ND 4.0 |
Radical thinking
At Loughbrickland, Mills came face-to-face
with the realities of the political situation, and its impact on religious
tensions, poverty and local landlord-tenant relations. The village was in the
heart of the countryside and populated by some 600 people,[14]
which he described as being mostly Presbyterian, with some Catholics and
Protestants.[15] This is
important since Mills arrived there soon after the Irish rebellion of 1798, and
the Act of Union (1801), which abolished the Irish parliament and helped build
momentum behind the cause of Catholic Emancipation. Both events created
upheaval and pervaded the thinking of disparate parts of the population.
Although large numbers of Irish people fought with the British against
Napoleon, there was much support for France, particularly amongst those who had
sympathised with the American revolution in the 1780s. This latter group
included certain classes of Catholics, city dwellers and especially, Ulster
Presbyterians.[16] Mills
was amongst this cohort, and his views had been sharpened during his time at
Edinburgh.
Edinburgh at the time was not just a place to
study medicine. Through the 1790s, it was a breeding ground for radical and
novel thinking, and the university was a centre for a specifically Scottish type
of Enlightenment thinking that promoted rationalism, humanism and empiricism.[17]
The ideas of Thomas Paine and his Rights of Man (co-written with
General Lafayette), were widely circulated and discussed, and many new radical
societies emerged that sought political and religious reform. Later in the decade –
just as Mills was graduating – societies of United Scotsmen emerged that
aligned with the United Irishmen.[18] It is highly
likely that Mills was familiar with Irish radical contemporaries like Thomas
Drennan who graduated from Edinburgh medical school twenty-one years before
Mills. In Dublin from the 1790s, Drennan was active in the Volunteer movement and the fight for an independent, reformed Irish
parliament, and was a key leader in the Dublin
Society of United Irishmen.[19]
We know that Mills admired Dr Alexander Crawford of Lisburn, since he called on
him to attend his mother in May 1805.[20]
Dr Crawford was well known and had an extensive medical practice; he was also a
radical and active Volunteer in 1793/4, was implicated in activities with the
French in 1794, and was arrested with other United Irishmen in 1796.[21]
Loughbrickland realities
The young Thomas Mills absorbed these radical, new ideals and they underpinned his perspective and observations on Loughbrickland. With its mix of religions, Loughbrickland was exactly the type of area that experienced repercussions from the 1798 Rebellion, which in many areas led to a decline in interaction and good feeling between Catholics and their neighbours.[22] In July 1805, he wrote ‘religion has a powerful influence on our civil and political opinions’, and observed ‘with regret’ that the longstanding animosity between all classes of Catholics and Protestants had erupted into open disputes. ‘The flame is only smothered’, he wrote, and very little would make the flames ‘blaze forth’.[23] He bewails the‘depraved’ men who sought to make religion ‘an engine of government’, for the ‘vilest and most base’ reasons.[24] Yet he was not truly a radical, at least in the Edinburgh style: while he sought reform, he believed that religion was fundamental to human development, and could not be easily laid aside.[25]
There are also elements of Lamarckian thinking
in Mills’ letters. Lamarck’s theory posits that a
person’s characteristics could be acquired by behaviour,[26]
and passed through to the next generation. The more radical thinkers, including a number of
medics at Edinburgh University, supported this,[27]
and threads can be seen in Mills’ writing. Mills wrote
that he saw a ‘great number of patients’ with asthma and consumption.
Consistent with his views on fever, he discounts lack of fuel, poor clothing, ‘mode
of living’ and the weather as causes. Rather, he attributes the illnesses
partly to ‘the intemperance and debauchery of our forefathers’, and cites
‘constant inter-marriage of families’ and a ‘long abstinence from animal feed
and other nourishing diet’ as contributing factors.[28]However,
Mills was not a true Lamarckian, in that he was not an atheist or
anti-Religion;[29] on the
contrary, he frequently mentions the value of religious thinking and
instruction as essential to morality, wisdom and
happiness. He could be seen to be Lamarckian in that he believed thatpeople could,
through their own exertions, advance their position and power.[30]
Many of Mills’ letters focus on the work habits and productivity of the people of Tartaraghan and Loughbrickland. He noted the highly-cultivated fields and neat, clean and comfortable looking cabins and he admired the work ethic of farmers who supplemented their farm income by weaving.[31] He also admired the capability and industriousness of women who worked at sewing, spinning, weaving and knitting, and engaged in making hay, digging potatoes, pulling flax and reaping the harvest.[32] He was realistic enough to realise that poor families, no matter how hard they worked, could often not earn enough to ‘provide themselves with the necessities, much less the comforts of life’.[33] Mills’ letters reflect a deep awareness of the unequal distribution of wealth between the land-owning and the tenant classes. He acknowledges that the wealth of people like himself, living ‘in the lap of luxury and pleasure’, depended on the very existence of a discontented tenantry, asking if it should be surprising that ‘such men become rebels’.[34] He even anticipates the potential of a French-style revolution if this is not addressed. He writes, ‘We will not discover, I fear, our real interest, ‘till fatal experience teach it to us - ‘till we taste a little of those sorrows that we have made others feel’.[35]
Overall, Mills' settles on education and
virtue as the best response to poverty and bigotry:[36]
a fairer, more equitable country could be built if young people were taught to
be ‘good citizens’, to ‘admire virtue and despise vice, and to be frugal,
industrious and sober’.[37]
He lauds the local people for sending their children to school,[38]
and conversely, considers the potential for ‘despotism and slavery’ if
property-owners are not well-educated.[39]
He goes so far as to call for a law to prohibit any man ‘unacquainted with the
Principles of Liberty’ from owning Property.[40]
In many ways, Mills appears less a radical and liberal than an Improver,
focusing on relieving poverty and achieving social and moral transformationthrough economic growth, education, and application of rational,
Enlightenment principals.[41]
Building a career
By September 1805, Mills had gained ‘health
and strength’, and anticipated returning to Dublin.[42]
Unfortunately, we do not know when Mills did settle back in the city. He got
married at a relatively advanced age[43] in 1814 to the 31 year old Augusta Sophia Hamill.[44] Little about the
couple’s personal life is known, except that they lived for a time at the
family home (possibly with Michael Mills) at 41 Dominick Street, Dublin, and by 1829, had moved a street away to 38 Granby Row. As a physician, Mills is recorded as treating patients in Dublin by
the mid-1810s. He is not listed in the 1809 annual report of Cork Street
hospital,[45] though
he may have returned to it in subsequent years, since he wrote a paper in 1813
based on case studies from there.[46]
In one noteworthy intervention, he was called as a witness to the declaration
of a miracle by the Catholic Diocese of Dublin. Mills had been treating Mrs
Mary Stuart, a religious sister in Ranelagh Convent, Dublin in 1823 for four
years prior to her ‘miraculous’ recovery.[47] Mills cannot have
liked the newspaper coverage, and especially the mockery
the
miracle declaration attracted from Protestant clergy
and other physicians. That incident notwithstanding, Mills kept close to the
Dublin medical fraternity and set out to establish his position, with the hope
of rising to the ‘head of my profession’.[48]
Some of the ambition that his brother Michael observed in him at the start of
his career remained,[49]
and Thomas took only a short time to achieve the wealth and ‘higher rank in
society’ that he sought.[50]
Mills published a series of papers and case studies over the years, includingessays on blood-letting, typhus, and on various diseases of the liver,
brain and other organs.[51]
By 1824, Mills had consolidated his position as a physician in Dublin. Mills’ ambition saw
him elected as joint vice-President and President of the
Association
of Members of the King and Queen’s College of Physician of Ireland in 1821,[52] and 1823[53]
respectively. While he clearly enjoyed some support from his medical colleagues within the College, Mills never became President or Vice-President of the College itself.
To Paris
Twenty-five years after his letters from
Armagh and Down, Mills travelled to France to alleviate his declining health.[54]
He may have gone to seek a change of air, to recover from overwork and
‘exertion of the intellectual faculties’, or for something more serious.[55]In his
letter of 3 September 1830, Mills writes that he
consulted with Dr Crawford– ‘a kind friend’ – who advised him to go on
to Nice. He followed the advice, but died there two months
later,on 6 November 1830. He was 57. The
Belfast Newsletter noted the death of this eminent and distinguished
physician who had made an extraordinary contribution to his profession. Mills,
it said, had been an ‘amiable and interesting companion, and a generous
friend’, and his death was ‘a source of deep affliction’ to a wide circle of
friends and colleagues.[56]
After his death, Augusta Sophia continued to reside at their home at 15 Rutland
Square East for at least the next five years;[57] in 1838, she
married Dr William Turner at Malvern Wells in Worcestershire.
Conclusion
While the letters represent a limited source, it seems reasonable to
conclude that Thomas Mills was a radical in his mind, a liberal in his heart,
and a pragmatist in his practice. His observations of country life are acute
and interspersed with the enlightenment ideas and radical principles he honed
at Edinburgh University, but his absorption of these principles and ideals was
selective, particularly in relation to his belief in the value of religion.
That he was sincere in his desire to address the plight of the poor is
evidenced by his taking a position at the Cork Street hospital, and his letters
are infused with sympathy and some empathy for the poor of County Down. He was
not extremist enough to be overtly public with his views; nor did his radical ideals
supersede his position in society or role as a physician, as in the case of
people like Drennan or Crawford. Nor, it turns out, was Mills’ espoused
ambition enough to see him rise to the very top of his profession as he had
wished. The Belfast Newsletter may have been correct in remembering him
as an eminent physician and amiable companion, whose ‘qualifications,
both of head and heart, were of no ordinary description’.[58]
The letters of Dr Thomas Mills are held in the archives of the Royal College of Physicians of Ireland Heritage Centre, and are part of the Thomas Percy Claude Kirkpatrick Archive, also known as the Dr Kirkpatrick collection.
Fiona Slevin
[1] Thomas
Mills, 3 September 1830, RCPI Kirkpatrick Archive, TPCK/6/3/5/26.
[2] The
French Revolution of 1830 took place between 26-29 July 1830, and resulted in
the abdication of Charles X; the king was replaced with a constitutional
monarchy with Louis Philippe on the throne. Lafayette was leader of the
opposition and had been a hero of the American Revolution of the late 1770s; he
co-wrote the Declaration of the Rights of Man and the Citizen,and was an outspoken advocate of religious
toleration and the abolition of the slave trade.Lafitte was also a member of the Chamber
of Deputies and led the development of finance and banking post-revolution.
Dupin (likely Dupin the Elder), was a magistrate, eminent advocate, and
President of the Chamber of Deputies for eight sessions.
[3]
Thomas Mills, 3 September 1830, RCPI Kirkpatrick Archive, TPCK/6/3/5/26.
[4]‘Letters
from Thomas Mills TPCK/6/3/5, in the Thomas Percy Claude Kirkpatrick Archive’,
n.d., The Royal College of Physicians of Ireland Heritage Centre.
[5] Harriet Wheelock,
‘My Dear Mich …’, RCPI Heritage Centre Blog, June 13, 2011; available
from http://rcpilibrary.blogspot.com/2011/06/my-dear-mich.html;
accessed 21 September 2021.
[6]‘Scottish Enlightenment’, British Council, July 2016; available from https://www.britishcouncil.org/research-policy-insight/insight-articles/scottish-enlightenment;
accessed 9 December 2021.
[7] Laurence
Brockliss, ‘Medicine, Religion and Social Mobility in Eighteenth- and Early
Nineteenth-Century Ireland’, in Ireland and Medicine in the Seventeenth and
Eighteenth Centuries, eds. James Kelly and Fiona Clark (London, 2016), p
77.
[8] Harriet Wheelock,
‘My Dear Mich …’, RCPI Heritage Centre Blog, June 13, 2011; available
from http://rcpilibrary.blogspot.com/2011/06/my-dear-mich.html;
accessed 21 September 2021.
[9]‘Cork
Street Fever Hospital and House of Recovery’, Cork Street Fever Hospital,
October 2015; available from http://corkstreetfeverhospital.ie/;
accessed 9 December 2021.
[10]
Thomas Mills, 1 May 1805, RCPI Kirkpatrick Archive, TPCK/6/3/5/2.
[11]
Thomas Mills, 1 May 1805, RCPI Kirkpatrick Archive, TPCK/6/3/5/2.
[12] John
Farmer, Patients, Potions & Physicians: A Social History of Medicine in
Ireland, 1654-2004, (Dublin, 2004), p71, 74.
[13]
Thomas Mills, 18 August 1805, RCPI Kirkpatrick Archive, TPCK/6/3/5/8.
[14]
Samuel Lewis, A Topographical Dictionary of Ireland, (Dublin, 1837),
lists the population as 617 people.
[15]
Thomas Mills, (n.d. possibly 1 or 2) July 1805, RCPI Kirkpatrick Archive, TPCK/6/3/5/5.
[16] Kennedy,
W. Benjamin, Catholics in Ireland and the French Revolution, Records of
the American Catholic Historical Society of Philadelphia, Vol 85, No.
3/4, 1974, pp 221.
[17]‘Scottish Enlightenment’, British Council, July 2016; available from https://www.britishcouncil.org/research-policy-insight/insight-articles/scottish-enlightenment;
accessed 9 December 2021.
[18]‘Scotland and the French Revolution’, The Scottish History Society,
n.d.; available from https://scottishhistorysociety.com/scotland-and-the-french-revolution/;
accessed 9 December 2021.
[19] A.T.Q.
Stewart, ‘William Drennan’, in Dictionary of Irish Bibliography,
October 2009, Royal Irish Academy, https://doi.org/10.3318/dib.002765.v1, accessed 9 December
2021.
[20] Thomas
Mills, 14 May 1805, RCPI Kirkpatrick Archive, TPCK/6/3/5/4.
[21] C.J.
Woods, ‘Alexander Crawford’ in Dictionary of Irish Bibliography,
revised December 2010, Royal Irish Academy, https://doi.org/10.3318/dib.002156.v2,accessed 9 December 2021.
[22]
John Gamble, edited by Breandán Mac Suibhne, Society and manners in early
nineteenth-century Ireland, Field Day, 2011, XXV.
[23] Thomas
Mills, 12 July 1805, RCPI Kirkpatrick Archive, TPCK/6/3/5/10.
[24]
Thomas Mills, 12 July 1805, RCPI Kirkpatrick Archive, TPCK/6/3/5/10.
[25]
Thomas Mills, 1 September 1805, RCPI Kirkpatrick Archive, TPCK/6/3/5/17.
[26] P.J.
Bowler, ‘Evolution, History Of’, in International Encyclopedia of the Social
& Behavioral Sciences, ed. Neil J. Smelser and Paul B. Baltes (Oxford,
2001), 4986–92; available from https://www.sciencedirect.com/science/article/pii/B0080430767030679.
[27]
Adrian Desmond, The Politics of Evolution: Morphology, Medicine, and Reform in
Radical London (Chicago, 1989), 5.
[28]
Thomas Mills, 29 August 1805, RCPI Kirkpatrick Archive, RCPI Kirkpatrick
Archive, TPCK/6/3/5/15.
[29]
Adrian Desmond, The Politics of Evolution: Morphology, Medicine, and Reform in
Radical London (Chicago, 1989), 4.
[30]
Adrian Desmond, The Politics of Evolution: Morphology, Medicine, and Reform in
Radical London (Chicago, 1989), 5.
[31]
Thomas Mills, 9 August 1805, RCPI Kirkpatrick Archive, TPCK/6/3/5/1.
[32]
Thomas Mills, 28 August 1805, RCPI Kirkpatrick Archive, RCPI Kirkpatrick
Archive, TPCK/6/3/5/13.
[33] Thomas
Mills, 30 August 1805, RCPI Kirkpatrick Archive, TPCK/6/3/5/16
[34]
Thomas Mills, 3 July 1805, RCPI Kirkpatrick Archive, TPCK/6/3/5/5.
[35] Thomas
Mills, 3 July 1805, p9- 10, RCPI Kirkpatrick Archive, TPCK/6/3/5/5.
[36]
Thomas Mills, 13 August 1805, RCPI Kirkpatrick Archive, TPCK/6/3/5/4.
[37]
Thomas Mills, 13-14 August 1805, RCPI Kirkpatrick Archive, TPCK/6/3/5/5.
[38]
Thomas Mills, (n.d., possibly 1 or 2 July 1805), RCPI Kirkpatrick Archive,
TPCK/6/3/5/5.
[39]
Thomas Mills, 18 August 1805, RCPI Kirkpatrick Archive, TPCK/6/3/5/9.
[40]
Thomas Mills, 18 August 1805, RCPI Kirkpatrick Archive, TPCK/6/3/5/9.
[41] W.
Forsythe, ‘The Measures and Materiality of Improvement in Ireland’, International
Journal of Historical Archaeology 17, no. 1 (2013), 73.
[42]
Thomas Mills, 4 September 1805, RCPI Kirkpatrick Archive, TPCK/6/3/5/19.
[43] Maria
Luddy and Mary O’Dowd, eds., ‘Meeting and Matching with a Partner’, in Marriage
in Ireland, 1660–1925 (Cambridge, 2020), 91–134; available from https://www.cambridge.org/core/books/marriage-in-ireland-16601925/meeting-and-matching-with-a-partner/EDDDE9E6E154ED7B3DAF063F99B75B9E;
accessed 9 December 2021.
[44]Probate
Record and Marriage License Index, 1270-1858, Keeper of the Public Records
in Ireland, (Dublin, Ireland), 745; available from www.ancestry.co.uk;
accessed 24 November 2021.
[45]Annual
Report of the Managing Committee of the House of Recovery, and Fever-Hospital,
in Cork Street Dublin, for the Year Ending 4th January, 1809 (Dublin,
1809); available from http://corkstreetfeverhospital.ie/wp-content/uploads/2015/10/1808.pdf;
accessed 9 December 2021.
[46]
An essay on the utility of Blood-Letting in Fever, (Dublin, 1813).
[47]Belfast
Newsletter, 22 & 29 August 1823; The Freeman’s Journal, 25
August 1823.
[48]
Thomas Mills, 1 May 1805, RCPI Kirkpatrick Archive, TPCK/6/3/5/2.
[49]
Michael Mills, 13 May 1824, RCPI Kirkpatrick Archive, TPCK/6/3/5/21.
[50]
Michael Mills, 13 May 1824, RCPI Kirkpatrick Archive, TPCK/6/3/5/21.
[51]An
essay on the utility of Blood-Letting in Fever, (Dublin, 1813); The
Morbid Anatomy of the Brain in Typhus Fever, (Dublin, 1817); Observations
on the Diseases of the Liver’ (Dublin, 1811 and 2nd edition
1821); An Account of the Morbid Appearances exhibited on Dissection in
various Disorders of the Brain, (Dublin, 1826); and An Account of the
Morbid Appearances exhibited on Dissection in Disorders of the Trachea, Lungs
and Heart, (Dublin, 1829).
[52]
The Freeman’s Journal, 11 May 1821.
[53]Transactions
of the Association of Fellows and Licentiates of the King’s and Queen’s College
of Physicians in Ireland. Volume 4, 1824, digitised by Wellcome
Library; available from http://archive.org/details/s3id13658270;
accessed 25 November 2021.
[54]Belfast
Newsletter, 26 Nov 1830..
[55] Richard
E. Morris, ‘The Victorian “Change of Air” as Medical and Social Construction’, Journal
of Tourism History 10, no. 1 (January 2, 2018), 4.
[56]Belfast
Newsletter, 26 Nov 1830.
[57] Pettigrew and Oulton, The Dublin Almanac and General Register Of Ireland,
1835, 308.
[58]Belfast
Newsletter, 26 Nov 1830.
Through a Glass Darkly: The Archive and the Imperfect Portrait of a Man
In this blog post, Hannah Kempel, a student on UCD's MA in History of Welfare & Medicine in Society, reflects on her personal responses to archival material relating to Dr Neil John Blayney (1874-1919) donated to the Royal College of Physicians of Ireland's Heritage Centre.
There’s a certain intimacy to archival documents, one that I’m not sure that I fully grasped before taking up this project. I had never really interacted with archival documents as part of a collection before. What little experience I had was in individual documents, either provided to me by professors or in database searches. The experience of interacting with a single archival collection is markedly different: deeper, more intimate, and more emotional.
We don’t always consider the emotional element of interacting with archives, but that has been my strongest response to this collection. Emotion in historical practice is controversial but useful. While some academics may believe it to be unnecessary or improper for historians, it can help us to move past our gut reactions and preconceived notions and draw out new understandings.[1] Beyond its use to the historian, empathy can also provide a way for us to engage more ethically with our sources.[2] We can treat our subjects as people with their own voices, not objects.[3]
This particular collection, the Neil John Blayney Collection at the Royal College of Physicians of Ireland (RCPI) Heritage Centre archives, only concerns one man: the eponymous Neil John Blayney. Far from being the calm and objective historian, I had many different feelings while sifting through Blayney’s documents: humour, annoyance, admiration. I was quite surprised by the depth of what I felt. My strong emotional response inspired me to dig deeper into Blayney’s experiences and motivations and provided me with a richer and wider experience.
Background
 |
| Dr Blayney, date unknown. Used with permission from the RCPI Heritage Centre. |
These are the barest of facts of Blayney’s life. They read more as a resumé than a biography and tell you little to nothing about what kind of man Blayney actually was. There is so much more to Blayney’s life, as there is for any person’s life, than the bare facts. Neil J. Brennan, Blayney’s grandson, took Blayney’s documents and pulled a much more colourful portrait of the man in his book Opening Dusty Boxes: The Life of a County Surgeon in Edwardian Ireland. His Blayney is an individualist who involved himself in politics and enjoyed playing football. He learned about these aspects and more from photographs, news articles, letters, and the inferences that he could make from what documents survived.[12]
Constructing Dr Blayney
How do you pull the person from the papers? There are almost one hundred items of Blayney’s in the Neil John Blayney Collection at the RCPI Heritage Centre. This collection consists of five categories of documents: those relating to his medical career, his personal life, his service in the First World War, medical records, and supplementary material collected by Neil J. Brennan.[13] At first glance this may seem rather comprehensive, but can one hundred items really encapsulate a person’s life? Twenty-six of those items are professional references.[14] Over a quarter of Blayney’s documents are written about him in a very specific professional context. What does that have to say, if anything, about who Blayney was?
In the book An Eye for Eternity Mark McKenna tells the story of Manning Clark, a famous Australian historian, and his wife Dymphna. Beyond telling the story of an influential man and his oft-overlooked wife, McKenna also digs deep into Clark’s self-conscious shaping of his own legacy through meticulous editing and choosing of his own documents. The sheer amount of records and the meticulous detail with which he documented and deliberately chose them indicate a great deal of effort was involved in Clark’s creation of his archival legacy.[15]
The question of what makes it into an archive and what does not can be quite fascinating. This can be a matter of policy, of concrete guidelines that lead to documents’ inclusion or exclusion from archives. For example, the RCPI Heritage Centre has a specific collection policy that is used to determine whether or not it will accept a donation, restricting its content to materials related to the history of medicine in Ireland.[16] The National Archives of Ireland goes one step further. Its policy is based on the National Archives Act of 1986.[17] What can or cannot be included in that archive is a matter of law.
Personal collections are somewhat different. An archive may choose to acquire them or not, but their creation is much more intimate and subjective than a collection created due to policy or law. Personal collections reflect the decisions and motivations of their creators. Manning Clark created his archival collection through a great deal of effort and time. He involved his family, especially his wife, in its creation.[18] Mark McKenna sees this management, which is interwoven into Clark’s biography, as Clark’s way of creating a second life for himself.[19]
Self-management and Self-reflection
The case of Manning Clark is in many ways an extreme example of managing one’s legacy. Clark was a historian who made his life’s work out of digging through papers in archives. He would have had a much wider understanding of the ways that personal documents can change and shape a legacy than Neil John Blayney, a county surgeon, might have had. This doesn’t mean that Blayney did not have a hand in creating his own archival collection.
Blayney’s collection has had a very different life than that of Manning Clark’s. By the time Clark created his collection and sent his documents to the Australian National Archive he was already a celebrity in Australia. He seems to have very explicitly desired to be written about in the future. He even left notes to future biographers in his diary.[20] Clark was desperate to be remembered. The Blayney collection’s path has been more circuitous. It was kept in the Blayney family’s possession, not as an archival collection used for research but as a set of “very dusty boxes” passed down to Dr Neil J. Brennan who donated it to the RCPI Heritage Centre.[21]
It doesn’t seem that Blayney ever planned for his documents to form a legacy for himself- at least not in the way Clark envisioned. Given that he died of a stroke at the age of 44 he likely didn’t foresee the end of his life any time soon, not like Clark’s anticipation in his old age.[22] This is not a collection borne out of a lifetime of study and management. We can then look at Blayney’s papers as a reflection of the documents he wanted to keep for himself, not for posterity.
What, then, did Blayney choose to keep for himself? Personal correspondence, handwritten notes, class notes, bills, letters of reference. Perfectly ordinary documents, the kind that anyone might have, that nevertheless reveal a life. Blayney’s papers reveal some of the twists and turns of his life and grant an insight into the practicalities of life as a doctor in the late nineteenth and early twentieth century. In diving into these documents one can reveal not just an example of the life of a middle-class county surgeon but the life of Neil John Blayney.
“Regarding Our Last
Correspondence”
 |
| The Irish Automobile Club premises, present day. Source: The National Inventory of Architectural Heritage. |
Blayney’s collection only contains the responses from the Club and a mechanic. He does not seem to have kept drafts of his letters in this case despite keeping other drafts.[25] As such we can only read the responses to whatever he wrote. The Club’s responses, mostly written by H.J. Clayton, appear more and more exasperated with whatever Blayney wrote them. The relationship between Blayney and the Club does not seem to have ended very amicably.
I bring up this case because it offers such an interesting glimpse into Blayney’s personality, yet Blayney’s own words are lost to us. The set of letters tell a particular narrative. The first letter profusely thanks Blayney for his contribution.[26] The next few letters give some details on the car’s breakdown within a month of the previous donation and discuss the Club’s inability to pay for repairs.[27] This begins a year-long dispute over who should pay for the car repairs.
This is a compelling sub-series for me. The letters, one-sided as they may be, tell a story of frustration on both ends. Blayney as viewed through Clayton’s letters seems frustrated with the Club for damaging his car, asking him to pay for repairs, and taking a long time in fixing the car. The Club, on the other hand, appears frustrated with Blayney for not paying and then leaving his car in their garage for a long time while the dispute was going on. There’s a certain sense of mundaneness in the letters, of a fairly common sort of argument over who should pay for something, even occurring as they did in the middle of a large international conflict. It’s such a human moment.
I had a very personal reaction to these letters when I first read them. James Lowry discusses this “affective response”, which he argues that users of archival material can employ in order to better “bear witness” to the people and events they are studying.[28] As I bore witness to this episode of Blayney’s life, I didn’t like what I saw. The letters in my experience of them do not paint Blayney in a very positive light. I found myself getting annoyed with him as I read the responses from the Automobile Club. Without Blayney’s own words to speak for himself, I could only view him through the words of an organization that he was in conflict with.
There is an archival concept called imagined records.[29] These are records that may have, could have, or we want to exist, but that we can’t find. We ascribe a lot of significance to these imagined records and we feel their loss. Imagined records can be incredibly personal for the person imagining them – creating their own affective response.[30] I’ve seen examples ranging from the medical records of a stillborn child to the records of colonised nations that were lost during decolonisation.[31] Compared to such painful events, some missing letters about car repairs may seem rather trite. Why compare them to much more important cases? Small instances can be used to conceptualise the wider problem – that archives can very rarely tell the whole story.
I can imagine the letters that Blayney sent. There are drafts of other letters and notes that he wrote in the collection.[32] From these I can piece out his writing style, his handwriting. I can guess some of the things that he wrote to the Club from Clayton’s responses. For example, Blayney seems to have wanted to know the details of exactly what parts of his car were worked on. There are several letters responding to his questions.[33]
I can’t know exactly what he said, however, and herein lies the trap. When I read the letters I felt annoyed at his imagined slights against the writers. Did that annoyance make me imagine his letters as more aggressive, more petulant than they might have been? Did I project my own experiences with similar disputes onto Blayney? This too I can’t know because I can’t read his letters. I can only imagine what might have been.
Mrs Blayney’s Medical Reports
 |
A nurse’s reports from the collection. Used with |
As a doctor, these records would make more sense to Blayney than to a layperson. These records could have had more value to him than someone who is not a doctor. But being able to read and understand a set of records is not the whole story. If Blayney had kept every set of medical records that he could get his hands on, the collection would be much larger than it is.
Blayney was not a meticulous record-keeper like Manning Clark. This means that there are fewer of Blayney’s documents that we can study, but conversely that also lends more weight to the documents that he chose to keep. If Clark’s collection is intentional and vast, Blayney’s is serendipitous and specific. His records seem to be confined to important documentation like income tax returns, professional papers, and items of personal interest. In which category would Blayney place the nurses’ records?
What were these thirty-three pages to Blayney? Important documentation relating to a family medical emergency? Perhaps, but likely not thought of in the way that he viewed an income tax return or furniture invoice. Something related to his profession as a doctor? Another document is a register of examination notes, so it’s not out of the realm of possibilities that he could have had a similar interest in keeping his wife’s nursing records.[37] However, Eily went to a different hospital than Queen’s County Infirmary, where he worked at the time.[38] These nurses’ reports would have had no direct bearing on his career. Blayney’s medical speciality also seem to have been tuberculosis, not what seems to have been pneumonia or influenza.[39] Or were these simply papers describing a difficult time in his wife’s life, made worse by the premature birth of his son shortly after her release?[40]
We can’t know for sure but we can guess. Perhaps we can see this as another very human moment. Blayney kept the details of Eily’s treatment in what was likely a very difficult time in both of their lives. Blayney seems to have cared about his wife, enough to push past his mother’s disapproval for their union.[41] It would make sense for him to be invested in her wellbeing. His exact motivations are not clear, but with this document we can approach a sense of the care that he felt for his wife and son.
This document is compelling for the questions that it raises. The archive can provide us with tantalising clues but rarely a smoking gun. Handed the concrete evidence of one man’s life I can only feel the weight of what is missing from Blayney’s records. Julia Laite wrote that “friendship… is so often missing from the historical record.”[42] Interpersonal relationships are often hard to pin down in the records we leave behind. We may be given clues but concrete proof eludes us.
Conclusion
While I’ve spent a good deal of words on what is missing from this collection, I’d like to spend a few more on what can be found. This collection is full of insights into the life of an average doctor in the late nineteenth and early twentieth century. Blayney’s papers were kept within his family’s hands for almost one hundred years before they were donated to the RCPI.[43] A lot can happen in one hundred years to a box of papers. Neil J. Brennan attributes the wealth of material still available to his mother and grandmother being “inveterate hoarders” and a great deal of thanks should be given to them for maintaining these documents.[44] I’ve spent a lot of time attributing quirks in the collection to Blayney’s choices, but Eily and Mary, Dr Blayney’s wife and daughter, deserve credit for their roles as family archivists. It is through their efforts that we now can study Dr Blayney’s life.
This collection is fascinating for its serendipity, both in what documents Blayney chose to keep and in its journey to the RCPI archival collections. The documents were far more likely to be destroyed or lost than to make their way into a traditional archival collection. Through this collection and other collections like it, we can see as if through a glass darkly aspects of the ordinary past that are so often forgotten.
Hannah Kempel
1. Katie Barclay, ‘Falling in love with the
dead’, Rethinking History 22, no. 4
(2018), pp. 459-473.
2. Michelle Caswell and Marika Cifor, ‘From
Human Rights to Feminist Ethics: Radical Empathy in the Archives’, Archivaria, 81 (2016), pp. 23-43.
3. Barclay, ‘Falling in love with the dead’.
4. Neil J. Brennan, Opening Dusty Boxes (Ireland, 2019), pp. 1.
5. Brennan, Opening Dusty Boxes, pp. 4-5.
6. Brennan, Opening Dusty Boxes, pp. 18.
7. Brennan, Opening Dusty Boxes, pp. 28.
8. Brennan, Opening Dusty Boxes, pp. 53.
9. Brennan, Opening Dusty Boxes, pp. 61.
10. Brennan, Opening Dusty Boxes, pp. 62.
11. Brennan, Opening Dusty Boxes, pp. 62.
12. Brennan, Opening Dusty Boxes, pp. viii.
13. Caiomhe Rehill and Harriet Wheelock, ‘Neil
John Blayney Papers’, RCPI Heritage Centre, pp. 1-30, accessed online,
https://rcpi-live-cdn.s3.amazonaws.com/wp-content/uploads/2021/06/Neil-John-Blayney.pdf,
3 December 2021.
14. RCPI Blayney Collection, Items 61-73, 75,
76, 78-88.
15. Mark McKenna, An Eye For Eternity (Carlton, 2011), pp. 32-33.
16.
https://www.rcpi.ie/heritage-centre/donations/, accessed 3 December 2021.
17. ‘Acquisition Policy 2018-2022’, An Chartlann Náisiúnta | National Archives,
pp. 1-16, accessed online,
https://www.nationalarchives.ie/wp-content/uploads/2019/03/Acquisition-Policy.pdf,
3 December 2021.
18. McKenna, An Eye For Eternity, pp. 32.
19. McKenna, An Eye For Eternity, pp. 553.
20. McKenna, An Eye For Eternity, pp. 32.
21. Brennan, Opening Dusty Boxes, pp. viii.
22. Brennan, Opening Dusty Boxes, pp. 62; McKenna, An Eye For Eternity, pp. 553.
23. RCPI Blayney Collection, Items 45-57.
24. RCPI Blayney Collection, Item 45.
25. RCPI Blayney Collection, Items 13, 14, 90.
26. RCPI Blayney Collection, Item 45.
27. RCPI Blayney Collection, Items 46-47.
28. James Lowry, ‘Radical empathy, the
imaginary and affect in (post)colonial records: how to break out of
international stalemates on displaced archives’, Archival Science, 19 (2016), pp. 193.
29. Anne J. Gilliland and Michelle Caswell,
‘Records and their imaginaries: imagining the impossible, making possible the
imagined’, Archival Science, 16
(2015), pp. 53-75.
30. Gilliland and Caswell, ‘Records and their
imaginaries’; Lowry, ‘Radical empathy, the imaginary and affect in
(post)colonial records’.
31. Gilliland and Caswell, ‘Records and their imaginaries’; Lowry,
‘Radical empathy, the imaginary and affect in (post)colonial records’.
32. RCPI Blayney Collection, Items 13, 14, 90.
33. RCPI Blayney Collection, Items 56, 57.
34. RCPI Blayney Collection, Item 44.
35. Brennan, Opening Dusty Boxes, pp. 62.
36. RCPI Blayney Collection, Item 44.
37. RCPI Blayney Collection, Item 97.
38. Brennan, Opening Dusty Boxes, pp. 35.
39. Brennan, Opening Dusty Boxes, pp. 36-7; Brennan, Opening Dusty Boxes, pp. 62.
40. Brennan, Opening Dusty Boxes, pp. 62.
41. Brennan, Opening Dusty Boxes, pp. 60.
42. Julia Laite, ‘The Emmet’s Inch: Small
History in a Digital Age’, Journal of
Social History 53, no. 4 (2020), pp. 963-989.
43. Brennan, Opening Dusty Boxes, pp. ix.
44. Brennan, Opening Dusty Boxes, pp. viii.












